Shadows and strength: Living, coping, thriving with sickle cell in Tanzania
TODAY, the world marks World Sickle Cell Day, a moment to draw attention to one of the country’s most pressing yet often overlooked health challenges—sickle cell disease (SCD). It is a condition largely misunderstood or unnoticed by the public, due to limited awareness and persistent social stigma.
Despite its widespread impact, SCD remains insufficiently prioritized within national health strategies. This year’s theme ‘Global Action, Local Impact’ urges countries to recognize the lived experiences of those affected and to translate awareness into meaningful, sustained action.
In Tanzania, where over 11,000 children are born with the disease each year—according to estimates from the Muhimbili University of Health and Allied Sciences (MUHAS) Sickle Cell Programme and supported by World Health Organization (WHO) regional data—the urgency for action is clear.
For many families, life with SCD means frequent health crises, prolonged hospital stays, limited access to effective treatment and the burden of social exclusion. The impact is not only medical—it is deeply personal, social and economic.
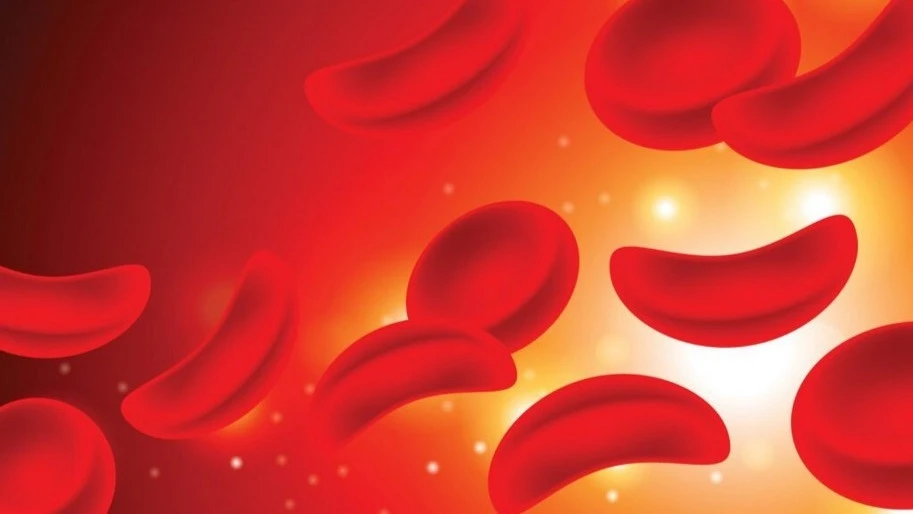
A genetic condition with a heavy burden
Sickle cell disease is inherited when a child receives a copy of the sickle cell gene from both parents. It causes red blood cells to change from their normal round shape into sickle or crescent shapes, which can block blood flow and reduce oxygen delivery throughout the body. These abnormal cells lead to frequent episodes of severe pain, anemia, organ damage, infections, and increased risk of stroke.
Tanzania is among countries where sickle cell disease remains a significant public health concern. According to MUHAS, the disease is responsible for the deaths of approximately 7 percent of Tanzanian children before their fifth birthday.
With roughly 20 percent of the population carrying the sickle cell trait—often without knowing it—the risk of having a child born with SCD remains alarmingly high.
Cultural misconceptions and societal stigma have historically made matters worse. Those who test positive for the disease or the trait have, in some communities, been shunned or discouraged from seeking medical care. But a growing movement is working to change this. MUHAS, through its sickle cell initiative, is bringing much-needed attention to prevention, education, and care.
Born into risk: The case for newborn screening
Early diagnosis has been proven to significantly improve the life expectancy of children with SCD. When a child is diagnosed at birth, preventive care can begin immediately—such as daily antibiotics, routine vaccines, and ongoing monitoring. These interventions greatly reduce the risk of life-threatening infections and complications in early childhood.
Newborn screening programmes have already been piloted in several regions, including Dar es Salaam, through collaborations between local and international institutions. These efforts have demonstrated positive outcomes in terms of early diagnosis and timely referral to care.
Expanding such programs to cover more regions presents an opportunity to further strengthen child health outcomes. Achieving this will require continued investment in testing kits, laboratory infrastructure, skilled personnel, public awareness campaigns, and sustainable funding mechanisms.
By increasing access to early screening, more children can receive the care they need from the very beginning—improving survival, reducing complications, and giving families the knowledge and tools to manage the condition effectively.
A lifeline in a pill: The promise of hydroxyurea
Hydroxyurea is a well-researched, low-cost oral medication that helps reduce the frequency of sickling episodes in people living with SCD. It lowers the need for blood transfusions, decreases pain crises, and improves overall quality of life. It is considered a frontline treatment and is recommended by WHO.
Tanzania has taken an important step by including hydroxyurea on the essential medicines list. As efforts continue to strengthen supply systems and raise awareness, ensuring wider availability across all regions—including rural and hard-to-reach areas—remains a key priority. In some cases, patients still travel long distances to access the medication.
Ongoing initiatives to improve supply chain coordination, expand training for health workers, and integrate hydroxyurea into national insurance benefits such as the National Health Insurance Fund (NHIF) will further enhance access and impact.
With consistent access to this vital medicine, the burden of sickle cell disease on families and the healthcare system can be significantly reduced, leading to healthier and more stable lives for those affected.
Pain beyond the body: The mental toll
While the physical symptoms of SCD are well-documented, its psychological impact is often ignored. Living with chronic pain, frequent hospital visits, and social stigma takes a heavy emotional toll. Many individuals with SCD experience anxiety, depression, and a sense of isolation.
Children with the condition may miss extended periods of school, affecting academic performance and social integration. Adults may find it difficult to maintain steady employment due to unpredictable health episodes. The psychological strain on caregivers—often parents or close relatives—is also significant.
Yet mental health services for people with SCD are almost nonexistent in most parts of the country. Integrating counseling services into SCD clinics, training healthcare providers to recognize psychological distress, and creating peer support groups could go a long way in addressing this often overlooked need.
As public understanding of mental health continues to grow, it is critical that these services be extended to individuals living with chronic conditions like SCD.
Myths, misunderstanding and stigma
Stigma continues to surround sickle cell disease in many Tanzanian communities. Some view it as a curse, a sign of weakness, or a punishment for wrongdoing. These beliefs lead to discrimination, delayed treatment, and psychological harm that can last a lifetime.
In some communities, individuals living with SCD may face social challenges—such as limited opportunities in education, employment, or marriage—due to lingering misconceptions and stigma. These misunderstandings can also discourage people from seeking testing or accessing the care they need. Continued public education is essential to addressing these barriers. These cultural barriers cannot be addressed by the health sector alone—they require a whole-society response involving trust-building, education, and empathy.
Religious leaders, community elders, educators and civil society organizations all have a role to play in dispelling myths and promoting accurate information. Community engagement programs and public awareness campaigns should be part of every regional SCD response plan.
Open dialogue is essential to breaking the silence that surrounds this disease.
The cost of care: A family affair
Managing SCD often requires regular medical visits, laboratory tests, medications, and at times, emergency care including blood transfusions. For many families, these costs are overwhelming. In regions where health insurance coverage is low, families must pay out-of-pocket, forcing difficult choices between healthcare and other basic needs, sometimes leading to dangerous delays in care.
The financial burden also includes transportation to distant facilities, loss of income due to caregiving responsibilities, and even the cost of food and accommodation when treatment takes place far from home.
To ease the burden on families, expanding SCD care within public health insurance and strengthening services at district hospitals are important steps. Establishing more well-equipped clinics would reduce travel time, improve outcomes, and lower costs.
Hope in science: Towards a cure
In recent years, medical science has made historic advances in the treatment of SCD. Two gene therapies—Casgevy and Lyfgenia—have been approved in high-income countries and show the potential for a functional cure. These therapies involve editing a patient’s stem cells to enable the production of healthy red blood cells, and the results so far have been remarkable.
However, these treatments are extremely expensive and depend on high-end healthcare infrastructure not yet available in most low- and middle-income countries. Their existence is both a breakthrough and a reminder of global health inequity.
Still, Tanzania is not standing still. The country hosts one of the continent’s most respected sickle cell research programmes at MUHAS. This programme has contributed significantly to global knowledge on SCD through its work on stroke prevention, malaria interactions and the use of hydroxyurea in African settings.
Continued investment in research, data collection, and local innovation will be key to long-term progress.
From awareness to action
On World Sickle Cell Day, the call to action goes far beyond raising awareness. It is a call for concrete steps from individuals, communities, institutions, and governments.
Getting tested for sickle cell trait should be routine—especially for couples planning to have children. Understanding your genetic status empowers informed decisions. Likewise, promoting prenatal and newborn screening programs ensures that care starts from the earliest stages and gives children a fighting chance at a healthy life.
Community members can contribute by engaging in open discussions about the disease, challenging harmful myths, and supporting local advocacy organizations. Faith groups, schools, and media platforms are powerful vehicles for change that can shape attitudes and reduce stigma from the ground up.
Donors and partners can play a critical role by supporting national programmes focused on medication access, research, and outreach. This includes investing in rural health systems, technology, and community education. Governments must show political commitment by increasing budgets for SCD care, training health workers, and improving supply chains for essential medications. Every stakeholder has a role to play.
When community leads, healing follows
This year’s theme underscores a vital truth as the power to transform lives lies not just in distant laboratories or large policy documents, but in the hands of ordinary people who choose to act. Health workers who educate, parents who advocate, leaders who prioritize, and survivors who speak out—they form the foundation of hope and resilience.
Progress begins with local courage—neighbours checking in, teachers learning more, health centers keeping essential medicines stocked, and young voices challenging stigma through storytelling. These small acts, multiplied across villages and cities, become a movement.
Sickle cell disease will not disappear overnight. But every life saved, every pain crisis prevented, every child who gets to attend school uninterrupted—that is progress.
World Sickle Cell Day 2025 is more than a commemoration. It is a moment to recommit, a time to elevate voices, bridge gaps and invest in health equity. It is a reminder that with coordinated action, sustainable investment, and a people-centered approach, Tanzania can lead the region in transforming the future of sickle cell disease.
Let us move beyond awareness. Let us act—with urgency, with compassion and with resolve.Heath
Top Headlines
© 2025 IPPMEDIA.COM. ALL RIGHTS RESERVED