Strengthening intersex healthcare in Tanzania: Progress, challenges and the call for self-worth

INTERSEX refers to a broad range of natural variations in a person’s sex characteristics—such as chromosomes, hormones, gonads, or genitalia—that do not fit traditional medical definitions of male or female bodies. These variations may be visible at birth, emerge during puberty, or only be detected later in life trough specialized medical tests.
In recent years, conversations about intersex people have gained visibility globally and increasingly within Tanzania. Although the subject remains sensitive in many communities, medical experts stress that intersex variations are more common than is widely assumed. Global estimates indicate that roughly one in every 4,500 babies is born with an intersex trait—equivalent to about 0.02 percent of all births.
At Muhimbili National Hospital (MNH), the rising number of intersex cases prompted the formation of a multidisciplinary committee of medical specialists in 2018. According to Consultant Pediatric Surgeon Dr Zaitun Bokhary, intersex variations are medically complex and cannot be understood or managed by a single specialist.
Intersex care involves much more than assessing external genital appearance. In most cases, it requires a comprehensive evaluation of hormones, internal and external anatomy, chromosomes, fertility potential, mental health and even legal considerations related to documentation and identity.
For this reason, MNH manages intersex cases through a coordinated team that includes pediatric surgeons, urologists, gynecologists, endocrinologists, psychologists, and legal experts.
Dr Bokhary emphasizes that every major clinical decision is made collectively. If even one specialist is unavailable, the meeting is postponed, underscoring the precision and caution required when determining treatment pathways.
The MNH Intersex Committee was created to address the growing number of patients and to provide structured, ethical, and evidence-based care. Since its formation, the committee has identified and supported more than 100 patients. However, Dr Bokhary notes that the country still lacks sufficient scientific documentation on long-term treatment outcomes.
To fill this gap, MNH is working to create a comprehensive national database that will support follow-up, track treatment progress, and strengthen understanding of the medical, psychological, and social realities faced by intersex individuals throughout Tanzania.
Among MNH’s success stories is the case of a 25-year-old woman who underwent cosmetic genital reconstruction at the hospital. Following treatment, she entered a stable relationship and later gave birth to a child through Caesarean section, as recommended to avoid complications linked to her earlier surgery.
This case, Dr Bokhary explains, illustrates that intersex people can lead full and fulfilling lives—form families, build careers, and participate fully in society when they receive appropriate care and support.
Challenges in identifying internal reproductive organs
One of the most demanding aspects of intersex management is identifying internal reproductive structures, which often requires sophisticated imaging. Some individuals may have a combination of male and female internal organs, making monitoring essential to avoid harmful or unnecessary interventions.
Diagnosis typically involves repeated MRI scans, ultrasounds, hormonal evaluations, and chromosomal analysis. These steps help ensure accuracy, safety, and individualized treatment for each patient.
Intersex people often face intense stigma. Many report being isolated, mocked, hidden by their families, or subjected to emotional trauma fueled by secrecy and fear. To counter these challenges, MNH enforces strict confidentiality protocols, ensuring patients' information is protected at every stage of care.
According to Dr Bokhary, this atmosphere of safety and respect is one of the main reasons intersex individuals feel comfortable seeking care at MNH.
MNH data indicates that about 70% of intersex patients are children, while 30% are adults. The high number of young patients suggests that many parents are unaware of intersex conditions or delay seeking help due to stigma. Some families, out of fear or confusion, initially turn to traditional healers, resulting in further delays in proper diagnosis and treatment.
Stigma often begins at home but extends to schools, religious institutions, and the broader community. This widespread discrimination discourages many intersex adults from seeking medical assistance until complications occur.
The high cost of treatment
Cost remains one of the biggest barriers. Many intersex patients lack health insurance, yet their treatment involves multiple investigations over an extended period. Previously, some essential tests were unavailable at MNH, forcing patients to seek services from private laboratories at high cost.
Thanks to advocacy from MNH specialists, the hospital now collects samples onsite and forwards them to partner labs. Efforts are also underway to ensure that key diagnostic tests are covered by health insurance schemes, easing access for patients from outside Dar es Salaam. According to Dr Bokhary, these improvements have provided significant relief to families that previously struggled to afford necessary care.
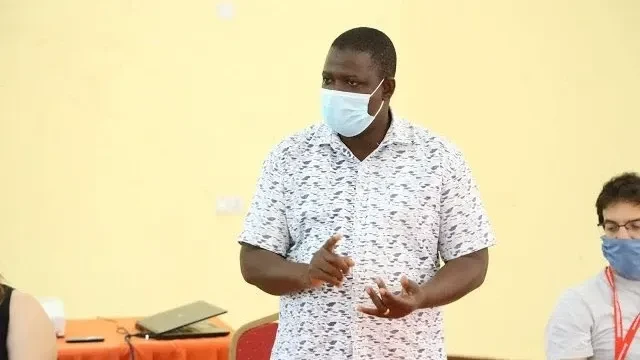
Tanzania Voice of Humanity (TVOH) CEO Baby John Musamba, who is herself intersex, stresses that stigma and discrimination remain major challenges nationwide. Gender-diverse individuals and their families often experience social exclusion driven by misconceptions based on physical appearance.
Baby highlights the serious issue of non-consensual medical interventions, explaining that some children undergo procedures without full understanding or informed consent. These interventions can lead to lifelong health complications and mental health struggles, yet hospitals rarely report the long-term outcomes.
She also notes that Tanzania lacks comprehensive legal protections for intersex people, leaving them vulnerable to discrimination. Limited awareness—from families to policymakers—creates a significant gap in understanding gender diversity.
Intersex individuals continue to face human rights violations, including derogatory labelling, harassment in public spaces, and discrimination in places of worship. Such experiences cause emotional distress that can negatively affect mental health.
Baby adds that healthcare barriers persist, with some providers asking inappropriate questions or offering unfriendly services based on a patient’s appearance, making it even harder for intersex people to access needed care.
As part of its mission, TVOH works on education and advocacy, government engagement, media outreach, and development of guidelines to support intersex rights. Its overarching goal is to increase awareness and push for policies that safeguard the dignity and well-being of gender-diverse individuals in Tanzania.
Building a supportive system for intersex individuals
Intersex conditions demand sensitivity, scientific expertise, and collaboration across medical and legal sectors. MNH is pioneering a model of care that upholds confidentiality, dignity, and comprehensive, multidisciplinary support.
As Dr Bokhary emphasizes, reducing stigma, raising awareness, and strengthening healthcare systems will enable intersex people to live fulfilling lives—defined not by anatomy but by their talents, aspirations, and humanity.
© 2025 IPPMEDIA.COM. ALL RIGHTS RESERVED