Tanzania’s brain centre: How Mloganzila is saving lives, building trust

FOR years, accessing specialist treatment in Tanzania—particularly for brain and spine problems—meant long journeys to a handful of major hospitals. That story is changing.
In 2017, Muhimbili National Hospital (MNH) opened its Mloganzila branch along the Morogoro highway. Initially designed to reduce pressure on Muhimbili’s main campus in Dar es Salaam, Mloganzila has since evolved into much more than a backup facility.
Today, it stands as a national hub for neurosurgery and a symbol of Tanzania's growing capacity to deliver advanced medical care through strategic investment, decentralization, and improved service delivery.
The numbers tell the story. The neurosurgery unit at Mloganzila now handles about 4,000 outpatients annually and performs 400 inpatient surgeries—a fourfold increase since it opened. This surge is not just about statistics; it reflects growing public trust in local health services and signals that government efforts to expand access to advanced care are working.
This article explores what Mloganzila’s success means—not just for patients, but for health workers, policymakers and the citizens whose taxes fund these life-saving services.
A new era in specialist care
In just seven years, neurosurgical inpatient numbers at Mloganzila have quadrupled, while outpatient visits have more than doubled. This growth reflects a fundamental shift in how specialist care is provided and accessed in Tanzania.
Previously, patients needing brain or spine surgeries—whether for tumor removal or trauma from road accidents—had limited choices: endure long waits at Muhimbili’s main campus or travel abroad at enormous personal cost.
That system was both unjust and inefficient. People living far from major cities faced longer waits and fewer options. Mloganzila was built to close that gap. Located just 30 kilometers from Dar es Salaam’s city center, it provides vital specialist care closer to home.
And it’s working. The hospital’s rapid growth aligns with the government’s broader goal of reducing costly foreign referrals, which, according to the Ministry of Health, drain more than TZS 10 billion from the national budget each year.
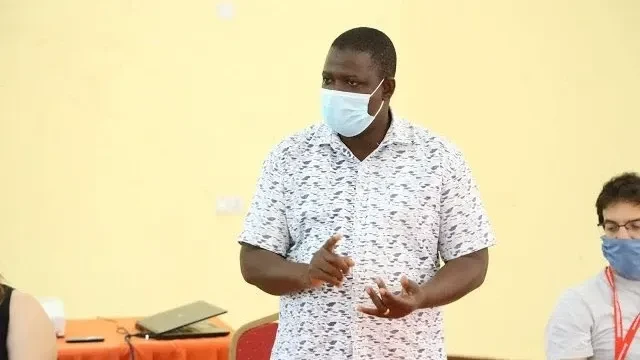
Building Tanzania’s own brainpower
Neurosurgery is among the most demanding medical specialties, requiring advanced equipment, highly skilled professionals, and coordinated teamwork. That Mloganzila now performs hundreds of brain and spine operations each year signals a remarkable achievement: Tanzania is building its own medical strength, reducing reliance on foreign treatment.
In recent years, the government has heavily invested in medical infrastructure—purchasing MRI and CT scanners, modern operating theatres, and fully equipped ICUs. But machines alone do not save lives—people do.
Between 2015 and 2023, the number of specialist doctors in Tanzania grew by more than 60%. Neurosurgery is now one of the fastest-growing fields in advanced medical training. Universities such as MUHAS, CUHAS, and KCMC have launched neurosurgery programs to produce 3 to 5 new neurosurgeons annually—a vital step forward for a country that had fewer than 10 neurosurgeons a decade ago.
Mloganzila serves not only as a treatment center but also as a teaching hospital, offering young doctors hands-on experience. Tanzania is also part of regional training networks like COSECSA, which promote surgical skills and cross-border learning. The real investment isn’t just in technology—it’s in talent, teamwork, and training.
Decentralization that works
For years, healthcare decentralization in Tanzania focused mainly on shifting administrative duties—not services. Mloganzila is changing that narrative.
This hospital shows what happens when decentralization is backed by real action. Instead of concentrating specialist care in Dar es Salaam or Mwanza, the country is expanding advanced services to more locations, bringing care closer to the people who need it.
Mloganzila is unique because it combines treatment and education. Medical students train in real hospital settings, learning from doctors who are actively treating patients. This integration of learning and healing benefits everyone—students, staff, and patients alike.
This approach is part of a national trend. In the past three years, Tanzania has built over 129 new district hospitals, 87 health centers, and upgraded more than 1,300 dispensaries. Over TZS 1.3 trillion has been invested to strengthen health services at the local level.
According to PO-RALG, more than 7,000 public health facilities now use Direct Health Facility Financing (DHFF), giving local health centers more control over budgets and decision-making. This system improves transparency and speeds up services.
While Mloganzila is managed nationally, it embodies this new model—where decentralization isn’t just a policy, but a lived reality that brings high-quality care directly to citizens.
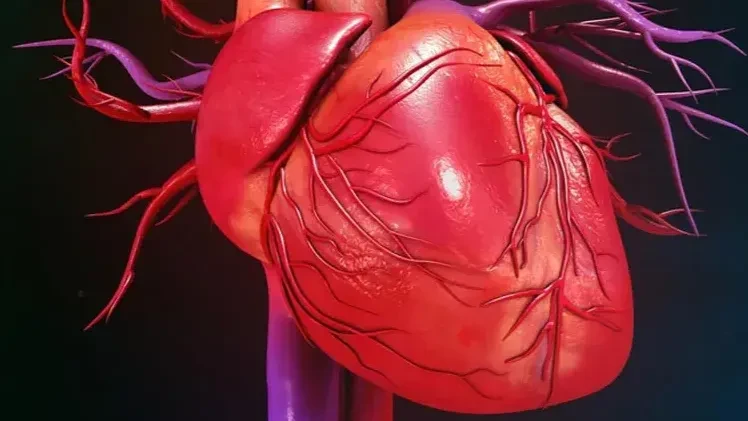
New Health Challenges: Brain and Nerve Diseases on the Rise
Tanzania’s health landscape is shifting. While diseases like malaria and HIV/Aids remain pressing, new challenges—especially brain and nerve conditions—are emerging.
Traumatic brain injuries (TBIs), mostly from road accidents and workplace hazards, are now among the leading causes of disability in Tanzanians aged 15 to 45, according to the World Health Organization (WHO). Strokes, epilepsy, and pediatric neurological conditions are also on the rise. With better diagnostics and public awareness, more people are getting timely diagnoses and treatment.
The Ministry of Health reports that over 192,000 Tanzanians were diagnosed with epilepsy in 2024/25, making it one of the country’s top neurological conditions. Stroke complications are now a leading cause of adult deaths in many regional hospitals.
This makes Mloganzila essential. By offering advanced brain care locally, patients no longer face months of waiting or the burden of costly overseas travel. Early treatment often means better outcomes, saving lives and reducing long-term disabilities.
Saving children’s lives through brain surgery
Beyond headline-making surgeries like tumor removals and trauma care, a quieter revolution is unfolding at Mloganzila—in pediatric neurosurgery.
Conditions such as spina bifida, hydrocephalus, and congenital brain malformations are now being treated early, giving children the chance to live full, healthy lives. Before 2017, many of these cases depended on visiting foreign surgeons or overseas referrals. Today, Mloganzila handles them routinely, proving that even the most specialized care can be built locally.
National initiatives—such as early childhood screening and improved maternal health programs—are helping identify at-risk children sooner. The Ministry of Health reports that improved antenatal and perinatal services have reduced preventable neurological birth complications, leading to better outcomes for infants needing surgery.
According to the Tanzania Demographic and Health Survey (TDHS 2022), skilled birth attendance has risen to 88 percent, up from 64% a decade ago. This has enhanced early detection of neural tube defects, which are among the most common reasons for pediatric neurosurgery admissions at Mloganzila.
What Mloganzila needs next
Building Mloganzila was a major milestone, but keeping it running at full capacity is the real challenge.
The hospital has become a trusted center for brain and spine surgeries, offering life-saving care closer to home. But sustaining this success requires consistent support: reliable supplies of medicine, well-maintained machines, ongoing staff training, and steady funding.
Health workers need fair pay, good working conditions, and professional development opportunities to stay motivated. Machines must be serviced regularly, and essential supplies must not run out.
There is also potential for Mloganzila to serve patients from neighbouring countries, positioning Tanzania as a regional leader in medical tourism—a move that could boost both health outcomes and the economy.
Mloganzila is living proof of what’s possible when vision meets investment. But keeping the momentum going requires commitment from government, health professionals, and citizens alike.
Beyond Mloganzila: A national blueprint
The success of Mloganzila raises an important question: why stop here?
Other hospitals—such as Benjamin Mkapa Hospital in Dodoma, Mbeya Zonal Hospital, and Kilimanjaro Christian Medical Centre—can follow the same path. The formula is clear: invest in infrastructure, partner with universities, expand diagnostic services, and support continuous medical education.
The Ministry of Health is already moving in this direction. Under the Health Sector Strategic Plan V (2021–2026), zonal hospitals are being upgraded to perform more complex surgeries. New operating theaters, diagnostic machines, and advanced training programs are being rolled out nationwide.
By 2026, the goal is to increase surgical capacity and reduce specialist care delays by 40%. By 2030, every region in Tanzania is expected to have at least two fully functional specialist units, supported by local training institutions and telemedicine services. This isn’t just a vision—it’s a plan already in motion.
Mloganzila’s transformation is not the end of the story—it’s the beginning of a new chapter in Tanzanian healthcare. Complex brain surgeries that once sent patients abroad are now performed locally, by Tanzanian doctors, with excellent results.
As Tanzania advances toward Vision 2050, healthcare must remain a top priority. Mloganzila is helping the nation achieve its goals of strengthening human capital, improving health infrastructure, and ensuring access to quality care for all.
With more domestic training, digital health expansion, and reduced surgical wait times, Tanzania is redefining what’s possible. Where “referral abroad” once meant fear and high costs, hospitals like Mloganzila now offer a different story—one of hope, trust, and national progress.
If this momentum is sustained, Mloganzila won’t just be a success story. It will be the blueprint for Tanzania’s healthcare future.
The author can be reached at judithjamestz@gmail.com
Top Headlines
© 2025 IPPMEDIA.COM. ALL RIGHTS RESERVED