Drug users: Peer-led drive effective in TB screenings

PEER-led approaches may significantly improve tuberculosis (TB) screening among people who use drugs (PWUD)—a population at high risk for TB but often overlooked by traditional health systems.
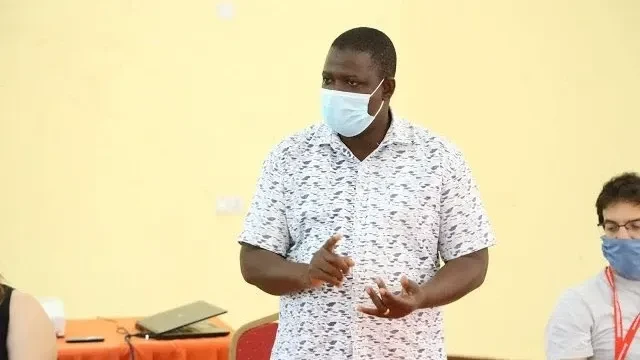
Dr Jerry Hella, a senior researcher at the Ifakara Health Institute (IHI), in an overview of the study where he was a lead researcher at IHI, said the new study conducted in Dar es Salaam has shown the unique role peers can play in bridging gaps in TB detection.
The study offers insight into the challenges and opportunities for community-driven health interventions in Tanzania, he stated, in the wake of the study being published in the Public Library of Science (PLOS One) journal, based in the University of California at Berkeley.
The study, based on in-depth interviews with 22 individuals—including peer educators, methadone clinic clients and community-based people who use drugs (PWUD) - found that peer-led TB screening is widely accepted and trusted by drug users.
Participants reported feeling more comfortable with service providers who share their lived experiences, helping reduce stigma and improve access.
"Having someone who understands what you go through makes it easier to talk about your health," one participant said.
The researchers identified several ways to strengthen peer-led TB efforts, including expanding mobile diagnostic services, integrating TB care into methadone clinics and offering small financial incentives to peer workers. Additionally, they recommended using chest X-rays and other symptom-independent tools to improve screening accuracy, as symptoms of drug use can sometimes mimic or mask TB, he stated.
Despite the promise of peer-led services, the study also pointed out ongoing barriers like stigma or inconsistent use of infection prevention measures (such as face masks). Other impediments are limited health knowledge and fears that TB treatment could worsen withdrawal symptoms among those using opioid therapies, he said.
Many participants were convinced that taking anti-TB medication could disrupt their methadone treatment, making them hesitant to start or adhere to treatment regimens, the researcher indicated.
The study was led by the National Institute for Medical Research (NIMR) with support from the Swiss Tropical and Public Health Institute at the University of Basel, the Muhimbili University of Health and Allied Sciences (MUHAS), the Drug Control and Enforcement Authority (DCEA), and the Muhimbili National Hospital (MNH).
To improve TB detection among PWUD, the researchers recommend increasing availability and coverage of mobile diagnostic units, incorporating tools like chest X-rays to complement symptom-based screening, along with launching peer-led awareness campaigns to tackle stigma and misinformation.
Using anti-TB drugs with fewer interactions with opioids is vital to avoid withdrawal and improve treatment adherence, he said in the summary, noting that tuberculosis remains the leading cause of death from a single infectious agent worldwide.
In 2023 alone, an estimated 2.7m TB cases were undiagnosed or unreported, on the basis of World Health Organization (WHO) data. The UN agency urges active case finding to close this gap—an approach that this study suggests can be more effective when led by peers, especially in marginalized communities, he further noted.
The findings provide a compelling case for scaling up peer-supported TB services in Tanzania and beyond, particularly through friendly drop-in centers that are accessible and acceptable to PWUD, he added.
Top Headlines
© 2025 IPPMEDIA.COM. ALL RIGHTS RESERVED