TB panacea: Consortium, IHI in trials for new cure
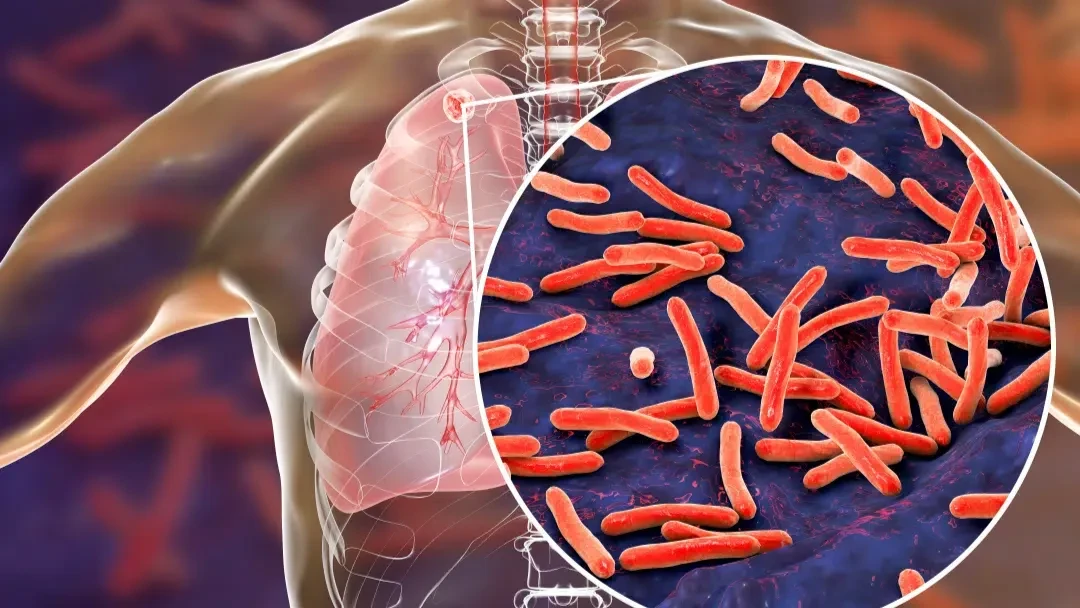
A clinical trial is bringing new hope to the fight against drug-resistant tuberculosis (TB), a recently published study has revealed.
The studies, published in ‘The Lancet Infectious Diseases’ and the Journal of Antimicrobial Chemotherapy, were led by the Panacea Consortium working with local scientists at the Ifakara Health Institute (IHI), which officials say it reflects the country’s growing involvement in global TB research.
Work on one of the world’s deadliest and most persistent infectious diseases was pursued in Tanzania and South Africa, with support from researchers and institutions in Tanzania, South Africa, Germany, the Netherlands, the UK, Sweden and the United States.
Initial results point to the possibility of safer, shorter and less toxic treatments, potentially transforming care for millions of patients, as drug-resistant TB has long defied easy treatment.
Patients face months or even years on harsh medications that can cause nerve damage, hearing loss and heart complications, while the new clinical trials signal a turning point.
It shifts from current treatments that are long, difficult and often toxic, with side effects such as nerve damage and serious heart complications.
Between 2021 and 2022, researchers tested two new drug combinations at five clinical trial sites in the two countries, to find safer, equally effective alternatives to the harsh medications currently used.
“The results are encouraging—these newer regimens showed strong treatment outcomes, with significantly fewer side effects,” a study summary asserts, indicating that treating drug-resistant TB will no longer be notoriously difficult.
In Tanzania, where TB remains a major public health concern, the demand for safer, shorter treatment is huge, and the latest research offers a glimpse of what that future could look like: No added heart risk from new drug combinations, the summary asserts.
The first study focused on cardiac safety—an ongoing concern with TB medicines. It found that combining standard drugs like bedaquiline, delamanid and moxifloxacin with either sutezolid or delpazolid did not increase heart risk, clearing the way for further trials using these combinations, it affirmed.
The second study tested sutezolid, a newer antibiotic. It improved the effectiveness of other TB drugs without causing major side effects, especially the nerve damage commonly seen with older drugs like linezolid.
The third study examined delpazolid, another potential alternative to linezolid. It worked well—particularly at a 1200 mg once-daily dose—and had a better safety profile.
“With further testing, delpazolid could become part of a new, global standard for treating drug-resistant TB,’ the study underlines.
The Ifakara Health Institute played a central role in the studies as its researchers like Dr Francis Mhimbira, Beno Huglin and Tresphory Zumba were deeply involved in study design, clinical trials and data analysis.
The wider result is that it isn’t just research conducted in Tanzania but IHI researchers leading the charge, the lead scientist noted, asserting that the team is helping to change the future of TB treatment worldwide.
The findings will help shape future recommendations from the World Health Organization (WHO) and guide national TB programmes in adopting safer, more effective therapies.
“Larger studies are now underway to confirm the results and move these promising treatments closer to approval,’ he added.
Top Headlines
© 2025 IPPMEDIA.COM. ALL RIGHTS RESERVED