Clinicians click links with skin disease gurus abroad

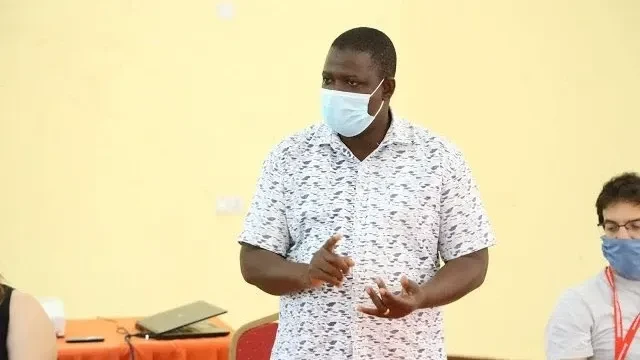
IN a district where access to dermatologists is scarce, local clinicians are turning to smartphones and internet technology to connect with specialists overseas.These links resulted from a study led by Dr Omary Juma of the Ifakara Health Institute (IHI) in Morogoro, working with Dr Michael Esson and Dr Karolyn Wanat of the Medical College of Wisconsin in the United States, researchers from the University of Iowa and clinicians at the Bagamoyo District Hospital.
The method now known as teledermatology enables medical staff in Bagamoyo to consult with U.S.-based dermatologists (skin disease experts) to remotely diagnose and treat patients—bringing expert care to communities that would otherwise go without.
In the study published in the Journal of the American Academy of Dermatology, IHI researchers and those of the medical college examined how often local clinicians' assessments aligned with those of remote dermatologists.
“We previously piloted the use of teledermatology and found it acceptable to patients. This study was aimed at categorising skin diseases in Bagamoyo and evaluate how teledermatology supports diagnosis and treatment,” the study summary indicates.
Researchers found strong agreement between local and remote clinicians for common conditions such as bacterial infections and eczema, while pointing at more complex cases—such as fungal infections and autoimmune diseases, it says.
Such cases often resulted in differing opinions, underscoring the challenges of diagnosing certain conditions without specialist training or laboratory support, it says, noting that as mobile technology becomes more accessible, telemedicine is emerging as a practical solution for underserved areas.
Still, the researchers caution that it is not a substitute for in-person care, stressing the need for ongoing training and support for frontline health workers.
“Sub-Saharan Africa faces a significant shortage of dermatologists, intensifying the burden of skin diseases,” the consultant asserts, pointing at teledermatology as offering a promising way to expand access to specialised care.
Their findings are aligned with global concerns, where a study on the global burden of disease shows skin conditions as the fourth leading cause of non-fatal diseases worldwide, affecting more than 4.6 billion people.
In February 2025, the World Health Organization (WHO) elevated skin diseases to a global public health priority when its executive board passed a resolution urging countries to integrate skin care into national health systems.
Countries need to invest in training, expand access to essential medicines and adopt innovations like telemedicine into routine medical care especially in rural and hard-to-reach areas, the UN agency said.
The resolution also highlighted the social and emotional impact of skin conditions, including stigma, discrimination and links to mental health issues like anxiety and depression.
The case study illustrates the potential and limitations of teledermatology, underlining that with greater international collaboration, investment in digital health and regular training of local clinicians, hospital centres like Bagamoyo could see vast improvements in dermatological care. For patients in remote communities, a smartphone may now be the first step to receiving the specialised care they deserve, the lead author intoned.
Top Headlines
© 2025 IPPMEDIA.COM. ALL RIGHTS RESERVED