‘ICU blood pressure patients more than twice likely to die’

PATIENTS with blood pressure under 90 mmHg were more than twice as likely to die during their hospital stay while those with dangerously low oxygen levels had a 62 percent greater risk of mortality, researchers have noticed.
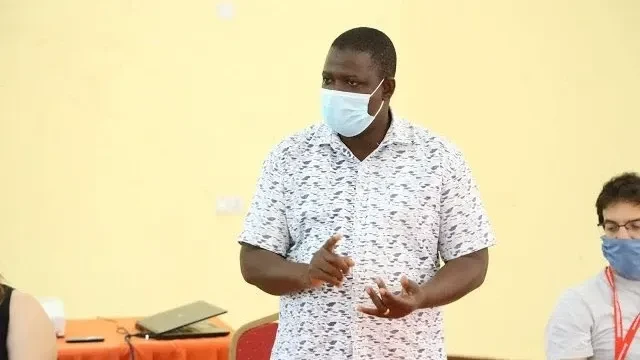
Dr Andrew Katende, lead researcher at the Ifakara Health Institute, makes this affirmation in a summary on a study of survival rates in high dependency hospital units (needing close observation) conducted in tandem with Basel University specialists in Switzerland.
The study focused on patient care and outcomes at the St. Francis Referral Hospital tied with the institute at Ifakara, Morogoro Region, whose results were published this week in the Public Library of Science (PLOS ONE) associated with the University of California at Berkeley.
It is one of the first studies to closely examine operations and survival rates within a high-dependency unit (HDU) in a rural sub-Saharan African setting, he said, noting that the research underscores the potential of HDUs in bridging the gap between general wards and full intensive care units (ICUs).
Prof Maja Weisser, one of the study supervisors, said in the summary that ICUs remain scarce and are typically found in urban centres, underlining that with proper investment HDUs can dramatically improve survival in rural settings where ICUs are simply not an option.
“But they must be equipped with essential tools—like oxygen delivery systems and basic monitors—and staffed with trained professionals,” he emphasized.
The study raised vital and at times alarming insights into the survival outcomes of critically ill patients in low-resource hospital settings.
Conducted from April 2023 to March 2024, the hospital’s high dependency unit (not having ICU facilities sufficiently) admitted 491 patients, where those aged 45 and above were mostly diagnosed with life-threatening conditions such as sepsis, stroke, aspiration pneumonia, acute heart failure and diabetes-related complications.
The findings highlight the stark challenges faced despite the dedicated efforts of clinical staff, as up to 30 percent of the patients died while in the HDU, and 37 percent did not survive the entire hospital stay, the summary exposition indicates.
“Mortality was especially high in patients suffering from sepsis (54 percent), aspiration pneumonia (65 percent), and stroke (51 percent),” it stated.
“These numbers reflect the severe nature of illnesses being managed in settings with limited equipment, personnel, and resources,” the lead researcher affirmed, noting that the study identified a number of clinical indicators associated with higher chances of death.
Older age—specifically patients aged 45 years and above—was a major factor. Others included critically low blood pressure, severely impaired consciousness and oxygen saturation levels below 90 percent, it explained.
Julie Rossier, co-lead author from the University of Basel, said that these clinical markers can help healthcare providers quickly identify patients at the highest risk. “Timely intervention is often the difference between life and death,’ she stated, describing the study’s findings as arriving at a critical moment.
Many African health systems are still recovering from the strain of the COVID-19 pandemic, while non-communicable diseases (NCDs) — including stroke and diabetes—are becoming leading causes of death across the continent, she asserted.
Dr Martin Rohacek, senior researcher and co-author, said that the research could inform national strategies on critical care, from triage protocols to staff training and infrastructure development.
The project represents a strong partnership between local and international institutions, drawing on local knowledge and global expertise to deliver evidence that is both contextually relevant and scientifically robust, he said.
Researchers hope their work will drive increased investment in critical care systems, especially in rural hospitals where preventable deaths remain common, he asserted.
Key data from the study are that total patients were 491 with median age as 46 years, where female patients were 53 percent of total. The mortality rate in HDU conditions was 30 percent during hospital stay and 37percent within its proximity.
Top diagnoses were sepsis (20 percent), hypertension (19 percent), diabetes (17 percent), acute kidney injury (13 percent) and heart failure (13 percent), the summary indicated.
Top Headlines
© 2025 IPPMEDIA.COM. ALL RIGHTS RESERVED