Bagamoyo lab achieves breakthrough in fight against malaria

MALARIA is endemic in most parts of the country. The disease quietly drains Tanzania’s economy year after year. According to the 2022 Tanzania Malaria Indicator Survey (TMIS), national malaria prevalence among children under five was 8.1 percent, down from 14.4 percent in 2015–16.
Lost workdays, hospital bills, and lower productivity cost the nation hundreds of millions of shillings annually.
Currently, scientists in Coast Region’s Bagamoyo District believe they may have found a way to stop the disease at its source: breeding mosquitoes that can’t carry malaria.
If the technology works, it could be one of the most cost-effective public health investments in the country’s history—and a transformation not just for public health, but the broader economic trajectory of the nation.
The initiative is part of the international Transmission Zero programme.
In a high-containment laboratory in Bagamoyo, researchers have achieved what once seemed impossible: breeding Africa’s first transgenic mosquito strain—modified so it can’t carry the Plasmodium parasite and can pass that trait to its offspring.
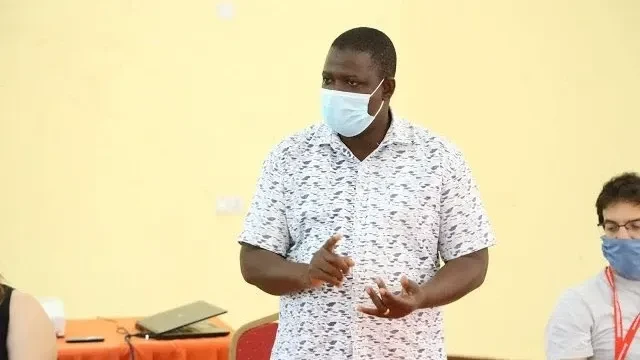
The breakthrough stands out because it was created on African soil by African scientists, as part of collaboration between Imperial College London, Ifakara Health Institute, Tanzania’s National Institute for Medical Research, and the Swiss Tropical and Public Health Institute.
“For decades, malaria has been a hidden tax on our economy,” says Dr Dickson Lwetoijera of the Ifakara Health Institute. “If we can cut transmission at the source, the returns will be both medical and economic.”
The technology promises a shift from nets, sprays, and drugs—which are increasingly compromised by insecticide and drug resistance—to a long-term, self-sustaining solution targeting the mosquito’s ability to transmit malaria.
Billions in potential savings
Globally, malaria killed nearly 600,000 people last year, with sub-Saharan Africa carrying the lion’s share—around 94 percent of deaths—and most of the victims are children under five.
The economic costs, however, are harder to quantify—but devastating. Across endemic regions, malaria drains health systems, burdens households, and reduces productivity.
In Tanzania specifically, malaria consumes around 3.4 percent of GDP, which translated in earlier years to approximately $240 million annually.
Households shoulder about 75 percent of this expenditure, with government and development partners covering the rest.
Additionally, over 1 percent of Tanzania’s GDP is devoted to malaria, equating to US $2.2 per person, and accounting for nearly 39 percent of the country’s total health spending.
Beyond direct costs, productivity losses from adult mortality are substantial—amounting to tens of millions of dollars in lost GDP.
Amplifying the economic toll, research estimates that average treatment and prevention costs for under-five malaria cases in Tanzania amounted to $132 million annually in 2009, escalating to $291 million when productivity loss from premature death was included.
If Transmission Zero succeeds, the gains could be enormous—hundreds of millions saved annually, fewer hospital visits, improved school attendance, a more resilient agricultural labour force, and a stronger, healthier workforce during planting and harvest seasons.
From lab to livelihoods
The project, envisaged as a $10 million investment, spans both scientific innovation and economic development.
It supports local scientific capacity, including the establishment of a mosquito transgenesis and infection facility with a biosafety level 3 laboratory at the Ifakara Health Institute. Importantly, it builds local ownership—a key factor for long-term sustainability.
Yet, the path from laboratory to field is not without hurdles.
As Dr Alexander Bailey of Imperial College notes, the challenge now is preparing for field trials—conducting rigorous risk assessments and transparent engagement with communities, policymakers, and regulators.
Moreover, gene drive technology, which pushes the altered trait through mosquito populations at rates far above natural inheritance, holds huge promise—but must be deployed cautiously and under robust regulation, with regional cooperation given mosquitoes cross borders.
A long-term economic gamble
This long-term genetic project began nearly six years ago. Today, infrastructure and regulatory frameworks are being established, and the government has extended larvicide distribution to all 184 local government councils as a complementary measure.
This dual approach—genetic innovation plus expanded larvicide—protects past investments and paves the way for future gains.
If successful, Tanzania could emerge as a regional leader, not only eradicating disease but exporting genetic technology and expertise—and unlocking new biotech revenue streams.
A future within reach
Malaria is not just a public health burden; it is an engine of poverty, educational setback, and economic stagnation.
Its impacts—up to 50 percent of hospital admissions, 40 percent of public health spending—are entrenched in daily life across endemic regions.
In Tanzania, the burden is most felt among young children, contributing to under-five mortality and long-term cognitive deficits that impair learning and productivity.
The Transmission Zero project offers a historic opportunity—not simply to eradicate malaria, but to unlock economic potential suppressed for generations.
If successful, the ripple effects could extend across the malaria belt, changing the destiny of countries long held back by this ancient scourge.
Top Headlines
© 2025 IPPMEDIA.COM. ALL RIGHTS RESERVED